Traumatic brain injury (TBI) is often a debilitating condition, caused by external injury or trauma which damages the brain.
This can disrupt the function of your organs and systems including the central and peripheral nervous system, the endocrine system, sensory systems, etc.
Statistics report that 70 million people in the world sustain TBI every year. 1.5 million of those happen in the US which has led to a total of 5.3 million Americans living with disability due to TBI alone.
The condition is often called “the silent epidemic” since in most cases it’s hard to detect brain damage even with modern imaging diagnostics and the condition remains undiagnosed.
Furthermore, patients themselves often neglect their head injuries, especially professional athletes or the military in the heat of action.
Unfortunately, even mild cases of TBI can have long-term consequences which appear months or years after the trauma. One of the possible consequences is endocrine dysfunction, most commonly manifesting as growth hormone deficiency (GHD).
Thus it’s important to get a proper diagnosis and assessment with timely treatment from an experienced physician.
In this article, you can learn more about the consequences TBI can have on your life and especially the dysfunctions of the endocrine system which commonly arise.
What is TBI?
TBI affects predominantly young and active people, and it’s twice more frequent in men than in women. The most common causes are traffic accidents, sports injuries, violence, and traumas related to military training or service.
Researchers classify the condition according to its severity in 3 groups: mild, moderate, and severe TBI.
Mild cases are the most common ones
The condition is defined as mild TBI if you have experienced only a short-term loss of consciousness and amnesia, or none at all.
On the other hand, moderate TBI always involves loss of consciousness for at least 30 minutes and amnesia that may range from one to several days.
Furthermore, severe TBI usually occurs when there is diffuse damage to the brain. Patients enter into a coma for longer than 24 hours.
Severe forms have a poor prognosis and many survive only several days or weeks after the injury. If they do, there is always long-term disability which significantly deteriorates the quality of life of these patients.
According to studies, permanent disability is thought to occur in 10% of mild injuries, 66% of moderate injuries, and 100% of severe injuries.
Physical and cognitive symptoms of TBI
The symptoms of TBI depend on the severity, the stage of the condition, and the part of the brain that is affected. The first two weeks after the injury are defined as an acute stage.
If you have mild TBI, you may experience several symptoms right after the trauma including headache, vomiting, dizziness, fatigue, ringing ears, blurred vision, and problems with muscle coordination.
Experts point out that you also may have transitory problems with mood, memory, concentration, and attention.
In addition to these symptoms, patients with moderate and severe TBI may experience convulsions, muscle weakness, dilation of one or both pupils, slurred speech, restlessness or unresponsiveness, and prolonged loss of consciousness.
The chronic stage of TBI begins after the first 3 months following the injury. According to evidence, common long-term symptoms of moderate and severe TBI include permanent changes in social behavior and cognitive capacity.
Patients often exhibit poor social judgment, with up to 61% being unable to identify, understand or describe emotions. Besides, the inability to sustain attention and reduced speed for processing information are quite common.
The consequences severely affect the daily life of patients, make them heavily dependent on specialized care and reduce their quality of life.
TBI also often leads to endocrine dysfunction since the pituitary gland can be easily damaged by external forces
Post-traumatic hypopituitarism (PTHP) may occur during the acute stage, especially if you have had severe injuries. It affects the production of corticotropins which may lead to life-threatening cortisol deficiency.
Research reports that the most common form of PTHP during the chronic stage is growth hormone deficiency. Interestingly, the risk of developing GHD is not related to the severity of TBI.
Thus, you may develop symptoms of growth hormone deficiency months or even years after sustaining relatively mild injuries.
Damage to the pituitary gland after TBI
Scientific evidence reveals that PTHP is quite common amongst patients with a history of TBI. It’s estimated to affect 15-68% of all cases of brain injury.
According to scientists, the pituitary is more prone to damage during TBI than other parts of the brain. Due to the unique location and the complexity of the blood vessels that surround it.
Currently, the exact pathophysiological mechanism of PTHP is unknown but researchers have several theories. The most prominent one is that PTHP is caused by damage to the blood vessels which cuts the blood supply to the gland.
If the TBI is accompanied by a rapid drop in blood pressure, this may also lead to infarction and damage to the pituitary gland.
In addition, there might be direct damage to the stalk of the gland due to the mechanical forces during TBI which disrupts the integrity of the neurons that connect it to the hypothalamus.
The TBI may also damage the blood-brain barrier and result in an autoimmune reaction and inflammatory response towards the pituitary gland. Antibodies against the gland are commonly detected in PTHP patients.
Usually, the anterior pituitary is most commonly affected. Due to the damage, the gland may cease production of several hormones including growth hormone, gonadotropins, adrenocorticotropin, and others.
GHD is the most common form of PTHP in the chronic stage of TBI
According to a meta-analysis of 29 studies, the incidence of growth hormone deficiency affects about 22% (range 2.7% to 63.6%) of all patients with brain injury.
Its symptoms are typical for growth hormone deficiency. Regardless of the cause, GHD is associated with loss of lean body mass, a buildup of abdominal fat, decreased bone density, cardiac problems, chronic fatigue, and poor quality of life.
Despite that fact, one trial reported that patients with TBI-related GHD are diagnosed on average 2.5 years later after the primary onset of disease when compared to other causes of growth hormone deficiency.
What other conditions can TBI cause years later?
Other long-term conditions which may occur due to TBI include:
- Post-traumatic epilepsy
- Parkinson’s
- Dementia (chronic traumatic encephalopathy and Alzheimer’s)
Movement disorders such as tremors and uncoordinated muscle contractions are common during the acute phase of moderate and severe TBI. The risk of seizures also increases with the severity of the injury.
Patients with seizures during the acute phase are likely to develop post-traumatic epilepsy. According to research, the incidence of epilepsy varies between 2-30% depending on the severity of TBI.
Parkinson’s is another neurodegenerative movement disorder that may occur due to TBI. Even mild injuries can lead to a 56% higher risk of developing Parkinson’s in veterans and the risk increases with the severity of the trauma.
The most common condition which may occur due to TBI is dementia. Repetitive brain injuries can lead to a specific type of dementia called chronic traumatic encephalopathy (CTE).
The exact threshold of injuries required for CTE to occur is unknown but the condition is especially common amongst professional athletes.
For example, one study found the condition in 223 out of 266 deceased American football players. According to the scientists, the risk increases by 30% for every year played as a professional.
A meta-analysis of 32 studies, representing over 2 million individuals also indicated a possible risk between TBI and another type of dementia – Alzheimer’s. Yet, there was no significant association between the condition and TBI in women or severe injuries with loss of consciousness.
Diagnosis of traumatic brain injury
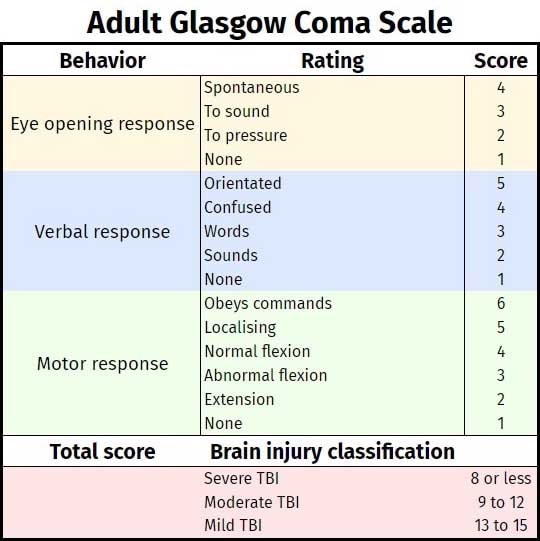
If you have TBI, your doctor will perform a neurological exam and start assessing the severity of your condition via a method called the Glasgow Coma Scale. Scores above 13 are usually classified as mild while scores under 8 are indicators of severe injury.
Once the initial assessment is complete, experts recommend that all cases of TBI undergo imaging diagnostics regardless of the severity.
The standard imaging method is computer tomography. It is highly informative and currently the most convenient method for use in emergency settings.
On the other hand, MRI is less convenient for emergency use but may provide much more detailed information for subtle injuries, including mild cases of TBI.
Mild TBI which presents with complications as well as all moderate and severe injuries should undergo screening for endocrine dysfunction and pituitary damage.
Complications in mild injuries suggestive for screening include: cases in elderly people, repeated TBI (usually in athletes), skull fractures, symptoms that suggest possible endocrine dysfunction.
During the acute stage, patients should be screened for possible corticotropin deficiency
Once you are into the chronic stage, you should be screened at least twice for other deficiencies including GHD. Scientists recommend that pituitary function is examined 3-6 months following the traumatic event and then once again at 12 months.
In some cases, it’s recommended that GHD screening continues after the first year following TBI. There are cases of growth hormone deficiency occurring several years after the initial brain injury.
Treatment for TBI recovery
About 90% of mild TBI cases fully recover. The majority of them can return to their normal life and do not suffer from long-term consequences.
Moderate and severe injuries often require intensive treatment throughout the acute stage, followed by continuous rehabilitation during the subacute and chronic stages.
According to research, the PTHP is usually transient during the acute stage of TBI. Nevertheless, lack of cortisol due to corticotropin deficiency can be life-threatening and the condition requires timely intervention.
On the other hand, a GHD may develop months or years after the TBI and it’s usually permanent.
If the condition is confirmed by provocation tests, such as an insulin tolerance test, then patients should receive proper treatment as soon as possible. Studies report that delayed diagnosis and therapy of GHD post-TBI is associated with slower recovery.
Therefore, patients with GHD should receive continuous treatment using recombinant human growth hormone (HGH) injections.
Studies reveal that GH treatment can significantly improve cognitive rehabilitation in those patients and resulted in better vocabulary, verbal IQ, and total IQ than control subjects. The treatment administration does not differ from that of patients with GHD due to other causes.
Also, BPC-157 may be effective for TBI recovery. However, there is a lack of evidence on the effectiveness of BPC-157 for TBI recovery, so more research is needed.



 Request Appointment
Request Appointment